Our body is our first home, how we take care of our body now, we will enjoy more in our old age. And of course, reduce the risk of low back pain in older adults. Because caring about the body very late is much better than never start. Let say how much you can manage giving time to your body, cooking food is just to feed the body with energy, exercises are to boost your body stamina, and sleeping to relax your body.
So we are all pretty much to take care of our first home but need to be more precise in case of requiring the healthy one. Bones and disks issue in the spines can degenerate with time and create stiffness and perhaps soreness. But the low back pain is not compulsory to happen as a result of age-related if only we take care of our lifestyle.
Types of Lower Back Pain
There are many ways to categorize low back pain – two common types include:
Mechanical pain
This is a type of lower back pain that is generally caused due to stress and strain on the muscle of the vertebral column. Basically, the mechanical pain occurs due to the habits one has developed such as sleeping in a bad posture, unusual way of lifting or bending. This pain issue can be cured by performing some measures. Below are some of the points that might help in dealing with this pain issue.
- Proper bending and lifting technique
- Sleeping in a right posture
- Sitting in the right posture
- Using a comfortable chair that maintains the right posture
Radicular pain
Radicular pain is a type of pain that rises from the back and hip and goes into the legs and spine. It generally feels on one side of the body. It might be possible that this particular pain can occur without any particular reason. In that cases, the treatment centers on the symptoms of the pain and the overall health of the person.
Severe Lower Back Pain Symptoms In Older Adults
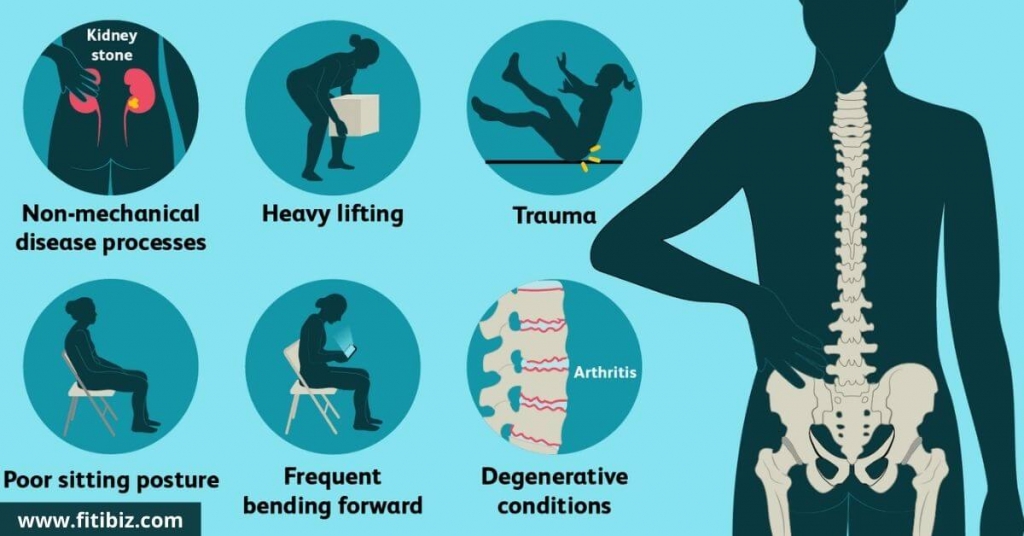
We all might experience back pain at some point in our lives but there are due to the wrong lifestyle we followed such as Smoking, being overweight, and poor eating habits, or due to some health conditions like cancer or spinal diseases. But the main cause for low back pain is nothing but AGING.
Usually, the pain takes its time during the morning and evening when a person feels the highest stiffness. Feel more of a pain when the injured area in the spine is pressed. Along with the feeling of aching and periodic pain while a person increases the body activity. Feeling the loss of flexibility and stiffness in the back.
Low back pain can happen for every age group but while a person across the age of 60 they are more prone to it which is due to the degeneration of the joints in the lumbar spine. Older adults are usually suffering low back pain because of Osteoarthritis and Spinal Stenosis.
Osteoarthritis and spinal stenosis are the two most common types of pain found in older people. So in this particular section, we are going to see the most common symptoms of lower back pain in old people. So below are given some of the common symptoms.
- Pain interrupting sleep
- Pain that starts in the early morning and stays the whole day
- Localized tenderness Aching, steady, or intermittent pain in the lower back stiffness or loss of flexibility in the back
- Sudden back pain
- Height loss
- Limited spinal flexibility
- Deformity and disability
The Common Reason For Facet Joint Osteoarthritis
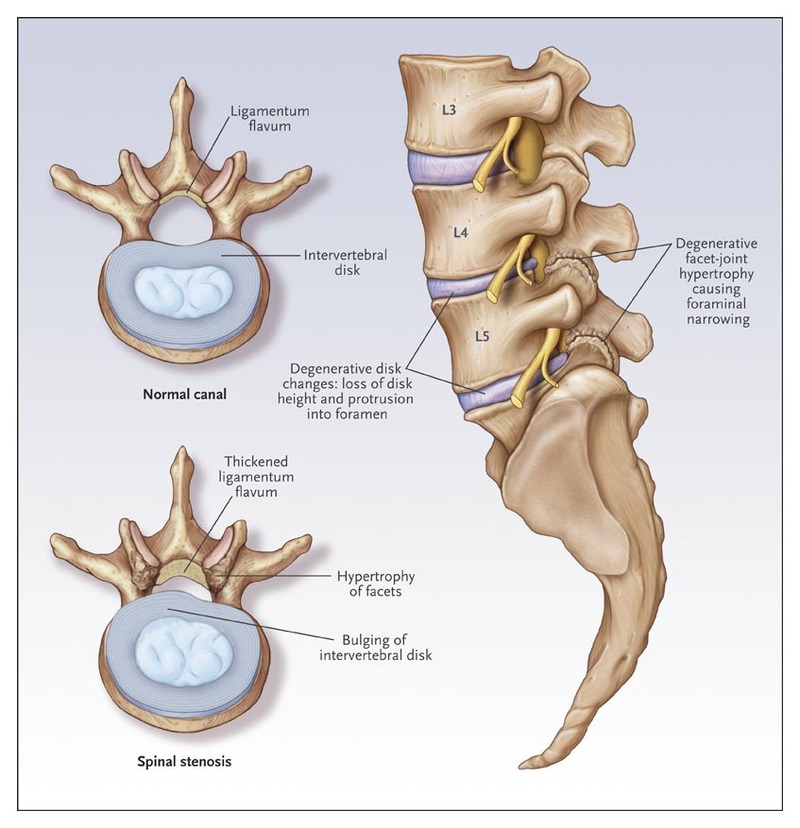
The spine contains individual bones which are called vertebrae and they are settled one on top of the other. Reduced bone mass, or osteoporosis, can even cause the vertebrae to weak to fractures. Also, The facet joints where each vertebra meets those vertebrae above and below start to degenerate, and create the other issue which is spinal arthritis.
Facet joint osteoarthritis, also known as degenerative arthritis or osteoarthritis of the spine, is a condition of degenerative that gradually increases over time. The injury happens because of the breakdown of the cartilage in the facet joints of the spine. Initially, the symptom can be intermittent, but later increase into more constant pain in the lower back, and ultimately causes sciatica as well to low back pain.
But can later develop into steadier pain in the lower back, and may eventually cause sciatica in addition to lower back pain. Osteoarthritis (degenerative arthritis) can cause the breakdown of cartilage between the facet joints. When the joints move, the lack of cartilage causes pain as well as the loss of motion and stiffness.
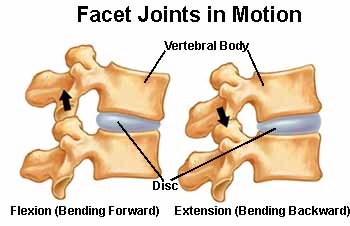
The facet joints are located in the back portion (posterior) of the spine. The joints combine with the disc space to create a three-joint complex at each vertebral level. The facet joint consists of two opposing bony surfaces with cartilage between them and a capsule around it that produces fluid.
The combination of the cartilage and the fluid allows the joint to move with little friction. However, facet joint arthritis causes the cartilage to breakdown and the joint movement is associated with more friction. The patient loses motion and as they get stiffer they have more back pain.
Lower Back Muscle pain from Osteoarthritis
The lower back pain very first starts in the morning. The pain starts as a normal pain in the morning but gets worsens as the day passes. In the daytime, the movement of the body causes fluid to better lubrication which starts getting the lubrication effects over as day passes and finally the pain starts in the lower back that can be even more worsen.
Facet Joint Anatomy in the Lower Back
Up and down the back of the spine, at each level, a couple of little facet joints interface the vertebrae the hard building squares of the spine, holding the spine together, and providing support. These joints, otherwise known as the zygapophyseal joints, are synovial, which implies they permit the spine to twist and curve in various ways.
Arrangement of the joint. A facet joint is shaped by the enunciation between combined hard projections called articular cycles. These cycles are situated at the back of every vertebra and interface adjoining vertebrae. For each plate space, there are two facet joints and a circle, which together structure a stand that makes the movement portion. The spinal nerves exit simply over the upper facet at each level.
The joint surfaces of the articular cycles are covered with ligament and typified by a thin, liquid-filled synovial layer to encourage smooth developments and forestall grating. A defensive covering of the joint. The joint is encircled by an external cause, which is intense, tough, and somewhat adaptable, and holds around 2 ml of joint liquid for grease. A limited quantity of fat enters and leaves the container during spinal developments for extra oil.
Pain can originate from the joint surfaces of a facet or the external case surrounding the facet joint.
Common Reason and Symptoms of Lumbar Spinal Stenosis
This particular type of pain creates the problem in the legs. Below are some of the most common symptoms of Lumbar Spinal Stenosis:
- Back pain
- Sensationless feet
- Issues in sexual activities
- Weakness in legs
Common Reasons of Lumbar Spinal Stenosis
Well, the most common cause of this Lumbar Spinal Stenosis is the wearing and tearing of joints as gets older. This issue generally occurs in the older ages. That is the reason generally people above 50 years faces this problem. Also, women are most likely to affected by this issue. There can be some other common reasons too for this particular problem. Below are given some other common reasons for this problem.
- Narrowing of the spinal canal
- Injured spine
- Tumor in spine
- Bone disease
- Surgery of the spine that were made in past
Symptoms of Facet Joint Osteoarthritis
Initially, the low back pain is along with the leg pain that happens while walking and standing straight and it combined with either of these problems:
- Not being able to walk for a long due to the pain in the leg.
- Lower back pain reduces after sitting for a while.
- Pain has fluctuated sometimes very intense and sometimes mild pain.
- Feeling of tingling, weakness, and numbness that spreads from the low back to the buttocks and legs.
The Possible Reason That Can Cause Spinal Compression Fracture
Usually, the likelihood of compression fracture can happen due to any sudden onset of low back pain in adults above the age of 50. like, women with their post-menopausal who have osteoporosis, and women or men after long-term corticosteroid use. For a person who has osteoporosis, the issue can get trigger even with a small amount of force give to the spine, such as a sneeze that can cause a compression fracture.
Less Likely Causes of Severe Lower Back Pain
Other reasons that it may cause the lower back is listed down, though they are not as common as the above mentioned one but still can cause the problem.
- Infection
- Fibromyalgia
- Piriformis Syndrome
- Spinal Tumor
- Coccydynia
- Ankylosing Spondylitis
All of these causes require room to talk about but meanwhile, this article is more or less concentrated on the causes and the common issues. As was discussed at the starting of the article, a person’s attitude and situation towards the body have the main impact on the duration and the level of pain. Likewise, those with a back injury, depressed people, and those under continuous stress are more porn to chronic pain. While patients with less complicating psychological problems and less stress are the ones who improve faster.
Physical Medicine To Relieve Extreme Lower Back Pain
Low Back Pain can be chronic or acute and according to the stage of the problems, there are different remedies given by physicians to get rid of the pain which can be medications, physical medicine, and even surgeries. Here we talk about physical medicines.
- Avoid those activities which can aggravate your pain
- Continue with your physical active therapy like stretching and passive ones like keeping ice, heat, body massage, electrical stimulation, and ultrasound.
- manipulation or Chiropractic therapy
- Yoga or Pilates, which is helpful to stretch and strengthen muscles.
Always you need to take your health seriously while noticing pain in your lower back you need to contact the physician and get the consultancy. Remember always curing in the first stage is easier than the last stage.
Final Note
So this was a small piece of knowledge about Lower back pain in elders. Take care of yourself and keep in touch with doctors. For more such amazing health-related blogs keep visiting us.



Write a comment
Your email address will not be published. All fields are required